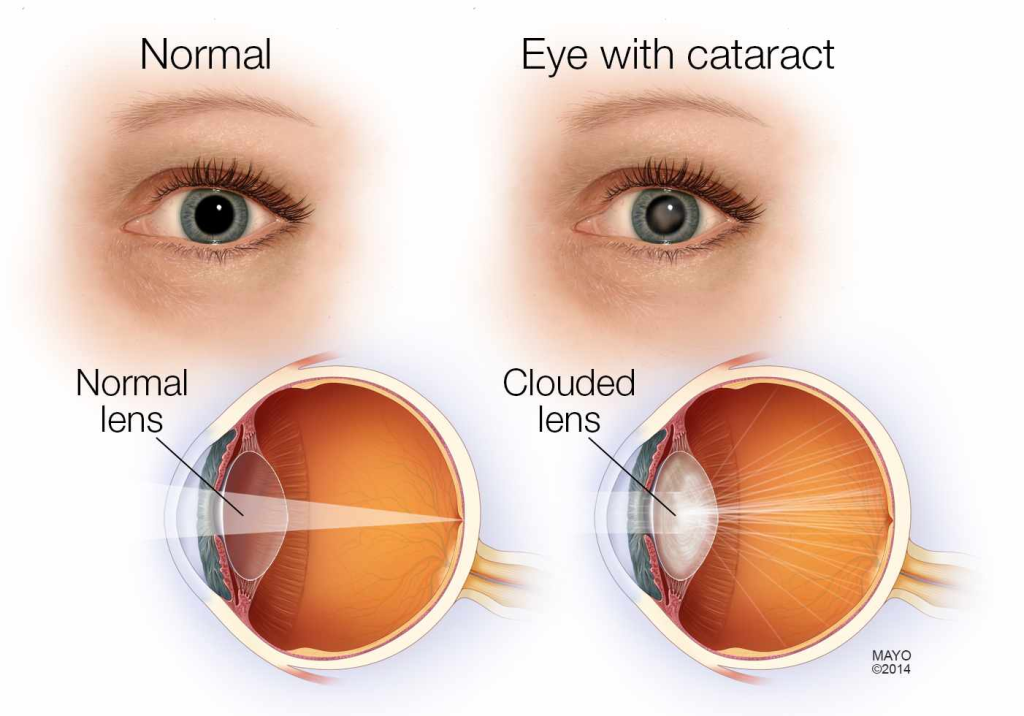
A cataract is an opacification of the crystalline lens that leads to progressive visual impairment. It is the leading cause of reversible blindness worldwide and is most commonly associated with aging.
Key Features of Cataract:
- Gradual, painless loss of vision
- Glare and halos around lights (especially at night)
- Reduced contrast sensitivity
- Absence of pain, redness, or other inflammatory signs
II. Classification of Cataract
1. Based on Etiology
| Type | Causes & Risk Factors |
|---|---|
| Senile Cataract | Aging-related oxidative stress and protein aggregation |
| Congenital Cataract | Intrauterine infections (TORCH), metabolic disorders (galactosemia) |
| Traumatic Cataract | Blunt or penetrating eye injuries |
| Metabolic Cataract | Diabetes, Wilson’s disease, hypocalcemia |
| Toxic Cataract | Steroid-induced, radiation exposure |
| Complicated Cataract | Due to uveitis, glaucoma, retinal detachment |
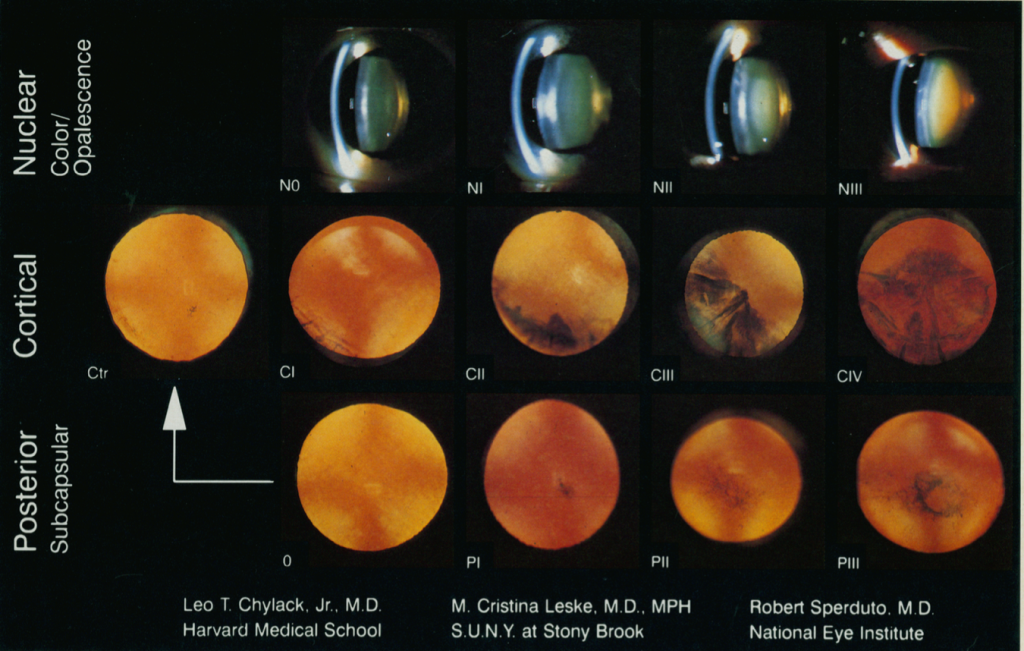
2. Based on Morphology
| Type | Features |
|---|---|
| Nuclear Cataract | Hardening and yellowing of lens nucleus, leading to myopic shift |
| Cortical Cataract | Wedge-shaped opacities in cortical fibers, often causing glare |
| Posterior Subcapsular Cataract (PSC) | Opacity near posterior capsule, worse in bright light and near vision |
| Christmas Tree Cataract | Multicolored opacities seen in myotonic dystrophy |
3. Based on Maturity
| Stage | Features |
|---|---|
| Immature Cataract | Partial lens opacification, fundus still visible |
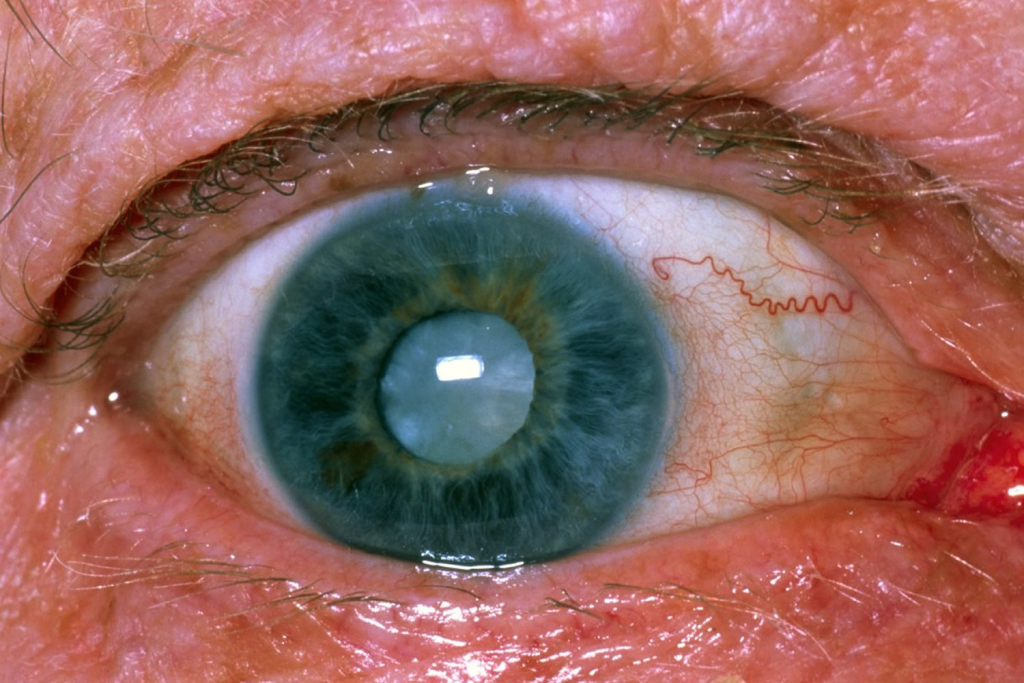
| Mature Cataract | Entire lens is opaque, no fundus view |
| Hypermature Cataract (Morgagnian) | Lens proteins liquefy, nucleus sinks |
III. Pathophysiology of Cataract Formation
1. Normal Lens Physiology
- Transparent due to organized lens fiber arrangement
- Maintained by Na⁺/K⁺ ATPase pump, keeping it dehydrated
- High levels of glutathione & ascorbic acid prevent oxidative damage
2. Mechanisms Leading to Cataract Formation
✅ Oxidative stress → Protein denaturation → Lens opacity
✅ Glycation of lens proteins in diabetes → Sorbitol accumulation → Osmotic stress
✅ Ultraviolet (UV) exposure → Free radical formation → Lens damage
✅ Steroid-induced inhibition of Na⁺/K⁺ ATPase → Water accumulation → Lens swelling
IV. Clinical Features of Cataract

1. Symptoms
🔹 Painless, progressive blurring of vision
🔹 Increased sensitivity to glare (e.g., while driving at night)
🔹 Monocular diplopia (double vision in one eye)
🔹 Frequent changes in spectacle prescription (especially myopia in nuclear cataracts)
2. Signs
✅ Lens Opacity on Slit Lamp Examination
✅ Absent Red Reflex (White reflex) in advanced cataract
✅ Brunescent (brown) or Morgagnian (liquefied) changes in late-stage cataracts
V. Diagnostic Evaluation
1. Visual Acuity Testing
- Snellen Chart: Measures degree of vision impairment
- Pinhole Test: Differentiates cataract from refractive errors
2. Slit Lamp Examination
- Assesses location and extent of lens opacity
- Retroillumination technique helps detect posterior subcapsular cataracts
3. Fundus Examination
- Essential to rule out retinal pathology in dense cataracts
4. Biometry (IOL Power Calculation)
- Keratometry + Axial Length Measurement → Determines intraocular lens (IOL) power
- Optical Coherence Biometry (IOL Master 700) → More precise for pre-surgical assessment
5. Contrast Sensitivity & Glare Testing
- Evaluates functional impairment in early cataracts
6. Ultrasound B-Scan (for Dense Cataracts)
- Used if fundus view is obstructed to assess retinal and optic nerve status
VI. Management of Cataract
1. Non-Surgical Management
✔ Early-stage cataracts – Adjusting glasses, anti-glare lenses
✔ Medical therapy (limited role) – Use of antioxidants like N-acetylcarnosine drops
2. Surgical Management (Definitive Treatment)
| Procedure | Indication | Technique |
|---|---|---|
| Phacoemulsification (Most Common) | Best for senile cataracts | Small incision, ultrasonic lens fragmentation, foldable IOL insertion |
| Extracapsular Cataract Extraction (ECCE) | Advanced, hard cataracts | Larger incision, nucleus removed intact, sutures required |
| Intracapsular Cataract Extraction (ICCE) | Rarely used | Entire lens removed, high risk of complications |
| Femtosecond Laser-Assisted Cataract Surgery (FLACS) | Premium option | Laser-assisted capsulorrhexis, lens fragmentation |
3. Types of Intraocular Lenses (IOLs)
| IOL Type | Advantages | Disadvantages |
|---|---|---|
| Monofocal IOL | Best distance vision | Requires reading glasses |
| Multifocal IOL | Good for both near & far vision | More glare/halos |
| Toric IOL | Corrects astigmatism | Expensive |
VII. Postoperative Care & Complications
1. Postoperative Care
✔ Topical antibiotics & steroids (to prevent infection & inflammation)
✔ Avoid rubbing the eye & strenuous activity
✔ Follow-up at 1 day, 1 week, 1 month
2. Complications of Cataract Surgery
| Complication | Description |
|---|---|
| Posterior Capsule Opacification (PCO) | Most common, treated with YAG laser capsulotomy |
| Endophthalmitis | Severe post-op infection, requires intravitreal antibiotics |
| Cystoid Macular Edema | Swelling of macula, managed with NSAIDs & steroids |
| IOL Dislocation | Lens implant shift, may need surgical correction |
VIII. Special Considerations
1. Cataract in Diabetic Patients
🔹 Develops earlier due to osmotic stress
🔹 More prone to posterior subcapsular cataracts (PSC)
🔹 Require tight glucose control before surgery
2. Pediatric Cataract
✔ Urgent intervention required to prevent amblyopia
✔ Primary IOL implantation in children >2 years
✔ Contact lenses or aphakic glasses in infants