Pulse examination is a crucial tool in modern clinical practice, providing valuable insights into cardiovascular hemodynamics, arterial stiffness, and systemic circulation. While manual palpation remains useful, advanced diagnostic modalities like ECG, Doppler ultrasound, and arterial tonometry allow for quantitative pulse analysis, aiding in disease detection, risk stratification, and treatment monitoring.
This discussion focuses on how clinicians can identify and interpret pulse abnormalities using these advanced techniques and includes clinical-level insights for better decision-making.
I. ECG (Electrocardiogram) and Pulse Analysis
A. How ECG Helps in Pulse Assessment?
An ECG provides a direct electrical mapping of the heart’s activity, which correlates with the pulse wave felt at the radial, carotid, or femoral arteries. Any discrepancy between ECG rhythm and pulse rate can indicate serious cardiovascular pathology.
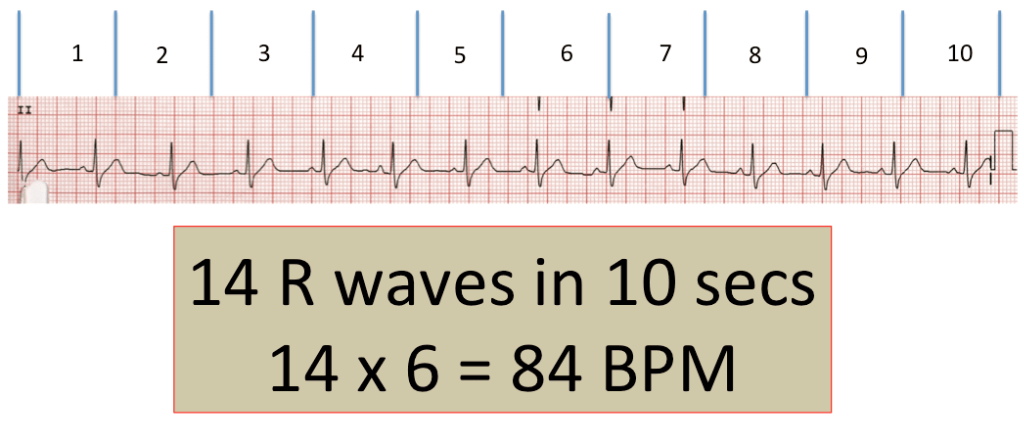
B. Clinical Identification of Pulse Abnormalities with ECG
| ECG Finding | Pulse Correlation | Clinical Significance |
|---|---|---|
| Sinus Tachycardia | Rapid, strong pulse | Seen in fever, hyperthyroidism, dehydration |
| Sinus Bradycardia | Slow, steady pulse | Common in athletes, hypothyroidism, sick sinus syndrome |
| Atrial Fibrillation (AFib) | Irregularly irregular pulse | Common in elderly, stroke risk factor |
| Complete Heart Block | Slow, regular pulse | Due to AV node dysfunction, pacemaker required |
| Ventricular Tachycardia (VT) | Weak or absent pulse | Life-threatening, requires immediate intervention |
| Pulsus Paradoxus (seen in ECG as electrical alternans) | Varying pulse amplitude with respiration | Seen in pericardial tamponade, severe asthma |
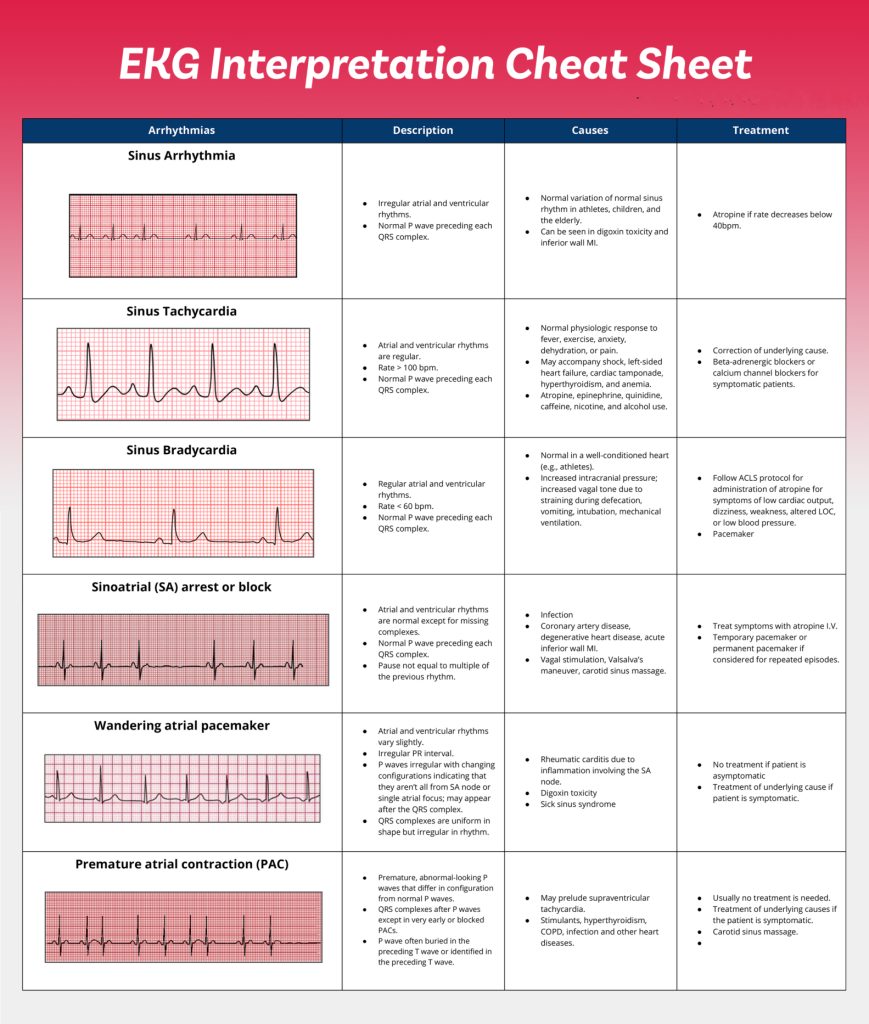
C. Advanced Interpretation of Pulse Findings on ECG
- Pulse Deficit: If the heart rate (ECG) is higher than the pulse rate (palpation), it suggests ineffective cardiac output due to arrhythmias like atrial fibrillation or premature ventricular contractions (PVCs).
- QT Interval Prolongation: Can be associated with torsades de pointes, which leads to an irregular pulse and syncope.
- ST Segment Elevation with Weak Pulse: May indicate acute myocardial infarction (MI) with cardiogenic shock.
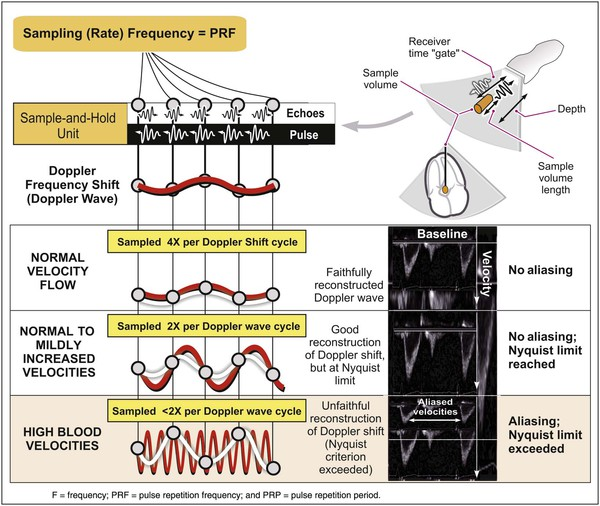
II. Doppler Ultrasound in Pulse Examination
A. How Doppler Ultrasound Helps in Pulse Assessment?
Doppler ultrasound provides real-time visualization of blood flow velocities, allowing clinicians to assess arterial patency, waveform morphology, and vascular resistance. It is highly useful in cases of suspected peripheral artery disease (PAD), deep vein thrombosis (DVT), and atherosclerosis.
B. Clinical Identification of Pulse Abnormalities Using Doppler
| Doppler Finding | Pulse Correlation | Clinical Condition |
|---|---|---|
| Triphasic Waveform | Normal, healthy arterial pulse | Normal peripheral circulation |
| Biphasic Waveform | Reduced elasticity, mild arterial disease | Early atherosclerosis, aging |
| Monophasic Waveform | Weak, diminished pulse | Severe peripheral artery disease (PAD) |
| Absent Waveform | No palpable pulse | Complete arterial occlusion (e.g., acute limb ischemia) |
| Turbulent Flow | Irregular pulse | Seen in arterial stenosis, post-thrombotic syndrome |
| Reversed Flow | Alternating pulse pattern | Seen in AV fistulas, aortic regurgitation |
C. Advanced Interpretation of Doppler Findings
- Ankle-Brachial Index (ABI): Used to assess PAD severity.
- Normal ABI: 1.0–1.4
- Borderline ABI: 0.91–0.99 (early PAD)
- Severe ABI: <0.40 (critical limb ischemia)
- Pulse Wave Velocity (PWV): Higher PWV indicates increased arterial stiffness and cardiovascular risk.
- Resistive Index (RI): Helps differentiate between arterial and venous pathology.
- High RI (>0.7): Suggests increased vascular resistance (seen in hypertension, renal artery stenosis).
- Low RI (<0.4): Seen in conditions like shock or sepsis.
III. Arterial Tonometry and Pulse Wave Analysis
A. How Arterial Tonometry Helps in Pulse Assessment?
Arterial tonometry is a non-invasive technique that records pulse waveforms using pressure sensors. It provides quantitative assessment of arterial stiffness, central blood pressure, and cardiovascular risk.
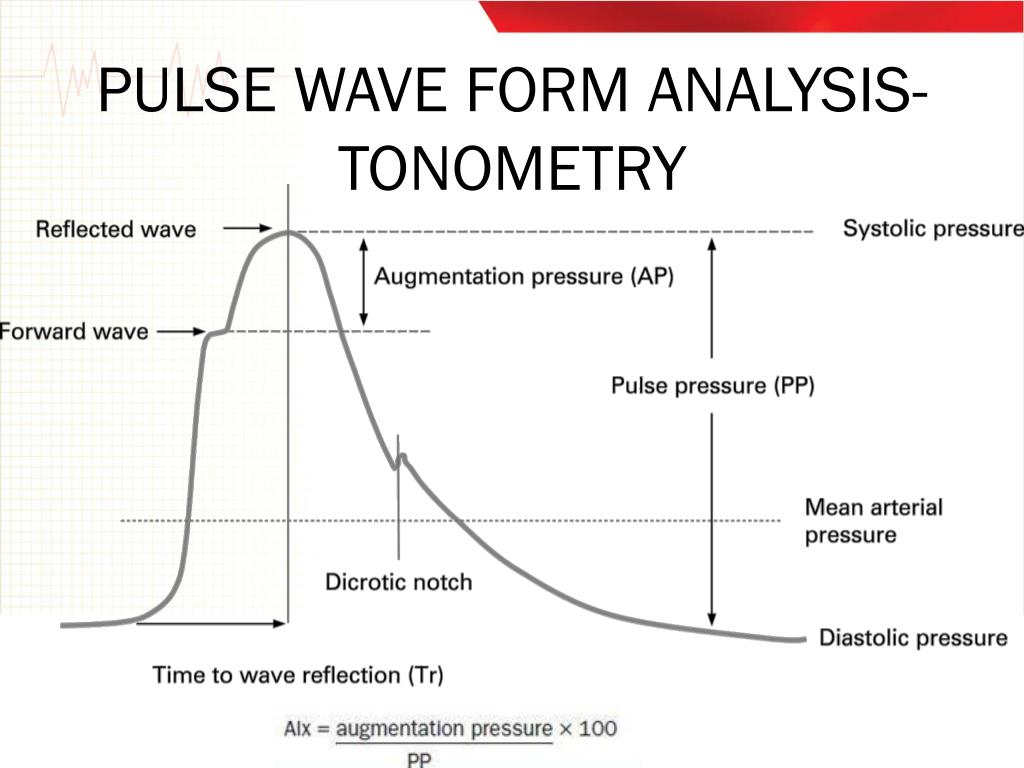
B. Clinical Identification of Pulse Abnormalities Using Arterial Tonometry
| Tonometry Finding | Pulse Correlation | Clinical Condition |
|---|---|---|
| Increased Augmentation Index (AIx) | High-resistance pulse | Hypertension, arterial stiffness |
| Increased Pulse Wave Velocity (PWV) | Rapid pulse propagation | Arterial aging, atherosclerosis |
| Elevated Central Aortic Pressure | High volume pulse | Cardiovascular risk predictor |
| Early Reflected Wave Arrival | Altered pulse waveform | Seen in diabetes, chronic kidney disease |
C. Advanced Interpretation of Arterial Tonometry Data
- AIx > 30%: Suggests increased arterial stiffness, common in hypertensive patients.
- PWV > 10 m/s: Strong predictor of cardiovascular mortality due to high arterial stiffness.
- Elevated Central Systolic Pressure (>130 mmHg): Indicates higher risk for stroke, MI, and left ventricular hypertrophy.
- Delayed Reflection Time: Seen in conditions like heart failure, where reduced arterial compliance leads to poor ventricular-vascular coupling.
IV. Case-Based Clinical Applications of Advanced Pulse Quantification
Case 1: A 65-Year-Old Male with Uncontrolled Hypertension
- ECG: Left ventricular hypertrophy with occasional PVCs.
- Doppler Ultrasound: Monophasic waveform in posterior tibial artery → Suggests severe PAD.
- Arterial Tonometry: AIx 45%, PWV 12.5 m/s → Suggests severe arterial stiffness.
- Diagnosis: Hypertension with advanced atherosclerosis.
Case 2: A 45-Year-Old Diabetic Female with Leg Pain
- ECG: Sinus tachycardia.
- Doppler Ultrasound: ABI of 0.6 → Moderate PAD.
- Arterial Tonometry: PWV 9.2 m/s, increased central pressure.
- Diagnosis: Diabetes-induced vascular disease with early cardiovascular risk.
Case 3: A 30-Year-Old Athlete with Syncope
- ECG: Normal sinus rhythm.
- Doppler Ultrasound: Triphasic waveform in all arteries.
- Arterial Tonometry: AIx -10% (low, which is normal in athletes).
- Diagnosis: Normal physiological adaptation, no pathological cause.
V. Conclusion & Clinical Takeaways
- ECG helps correlate pulse abnormalities with cardiac rhythm disorders (e.g., AFib, bradycardia).
- Doppler ultrasound is essential for detecting arterial occlusion, PAD, and assessing ABI.
- Arterial tonometry provides advanced insights into arterial stiffness and cardiovascular risk.
- Quantifying pulse characteristics enhances early disease detection, personalized treatment, and long-term risk assessment.